Here’s how vaccination helps prevent rotavirus
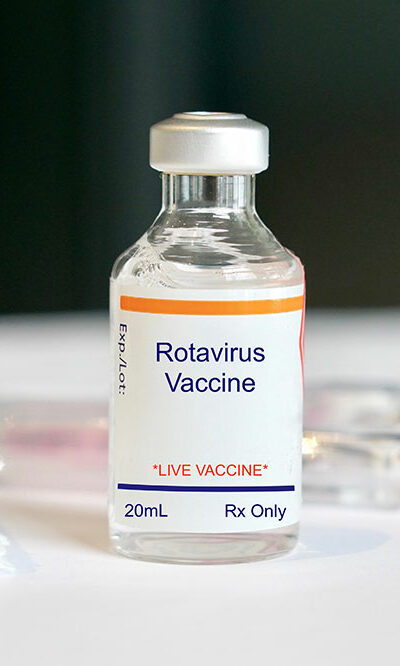
A rotavirus infection triggers diarrhea and vomiting in children. In fact, before the vaccine for this virus was developed, most children would be affected at least once by the age of 5. Doctors usually recommend giving children rehydration fluids to replenish all the water lost due to diarrhea. Other than that, there are no major treatments unless the infection triggers health complications linked to rotavirus. Herein, we discuss how getting a vaccine helps prevent rotavirus. Prevention of rotavirus Rotavirus is ranked among the top infectious diseases that majorly affects children under the age of 5. It remained the leading cause of diarrhea among infants up until 2006, when the first vaccine was introduced. Rotavirus is highly contagious infection that mostly spreads through hand and mouth contact. Along with a vaccination, good handwashing habits and overall hygiene will ensure that this disease doesn’t not rapidly spread. Adults must also ensure commonly touched surfaces are disinfected on a regular basis so that the child is not infected by contaminants on surfaces. Vaccination for rotavirus There are two approved vaccines that are given at a gap of two months. The first dose of the oral-drop vaccine is given to the child at the age of 15 weeks and both doses are completed before the child is 8 months old. The two approved vaccines for use are RotaTeq® The RotaTeq® vaccine is given three times: starting first at the age of 2 months, then at 4 months, and then 6 months Rotarix® Starting first at the age of 2 months and once at 4 months, the Rotarix® vaccine is given only twice. Note that the number of doses varies with these two approved brands. Statistics and studies indicate that vaccination protects almost 9 out of 10 children from severe form of the rotavirus disease.










